
As health care costs rise and high deductibles keep many from the doctor’s office, one West Michigan entrepreneur believes he has found a better way to provide health care.
Grand Rapids–based founder Jeff Boore is launching a startup aimed at making concierge-level health care accessible to everyone. His company, Aloe Health, uses a membership-based model known as direct primary care, where patients pay a monthly fee instead of relying on insurance.
Boore says the approach removes barriers and refocuses medicine on relationships rather than billing codes. The model is already gaining traction among employers and organizations seeking affordable care options for workers without insurance. Beginning in 2026, new federal rules will allow consumers to use Health Savings Account funds to pay for these memberships, a change Boore says could transform access to primary care.
Previously, Boore created Anjoy, a grocery subscription company designed to make healthy food more available. Now, with Aloe Health, he’s applying that same problem-solving mindset to health care. Rapid Growth caught up with Boore to talk about his latest venture and how he hopes to close the care gap through innovation.
Rapid Growth: You’ve spent much of your career in tech and startups, helping companies build new products across industries. What ultimately pushed you to start Aloe Health, and how did your background in innovation shape the way you’re tackling challenges in health care?
Jeff Boore: I have always been drawn to health care. I actually started pre-med in undergrad before realizing an entrepreneurial path might be a better fit. And honestly, not being able to stomach the sight of blood should have been my first clue.
Throughout my career, I continued to intersect with health care in different ways. I consulted for insurance companies, worked with a health care group moving toward a membership model, and saw the system through my wife’s experience as a doctor. But it still felt like the kind of system that would be hard to fix from the outside looking in.
That changed when I moved back to the Midwest and tried to find a new primary care doctor. Everyone was booking months out. When I finally got in, I had the stereotypical seven-minute visit. We did not have time to address everything, and then a “whelp, see you next year,” to end it. And that was it. At the same time, I was helping a family member navigate their care and struggling to find someone who could really spend time with them and understand what was going on.
Then I came across membership-based primary care, and it felt completely different. A consistent theme throughout my career has been building around what people actually need, and making sure the business model aligns with that. It’s something I love about membership-based primary care. Success depends on doing what is best for the member, not a third party.
At first, I thought, this is an amazing solution for people who can access it. And the more digging I did, the more I realized that if we built it the right way, we could make amazing health care available to everyone, while also improving the lives of those working in health care.
RG: Concierge medicine has long been seen as something reserved for a privileged few. How is Aloe Health using technology to make that level of personalized, high-quality care accessible to a much broader population?
JB: You are totally right. For a long time, concierge medicine felt reserved for a small group of people. And for them, the proof was in the pudding. It worked. The top 10 percent of income earners live about 10 to 15 years longer than the bottom 10 percent. Access to great primary care matters.
What we are doing is combining technology with a care model that is already proven, and making it accessible to more families and employers, not just a privileged few. This is a small part of what we have built. A much larger part is the incredible work direct primary care doctors are already leading, and part is just a math problem.
We know every dollar spent in primary care saves about $13 in downstream health care costs. However, the traditional system only works financially when people end up in high-cost care settings. In other words, it benefits from sick-care, not preventive care. So if we can shift those incentives and get more investment into primary care, the overall cost of health care goes down. A lot. Better access is not more expensive. It is what makes the whole system more affordable.
And it is just as important to talk about what we are not doing. We are not trying to use software or AI to replace the human side of medicine. Primary care works because there is a real relationship between providers and patients. We exist to enhance that, to remove administrative friction, and to support both members and physicians. It lets doctors spend more time caring for people and less time figuring out billing codes and insurance workflows.
The goal is simple: make care easy to access, personal, and proactive, and build a system where the economics reward keeping people healthy instead of reacting only when they are sick.
RG: How is your business using technology to reduce costs?
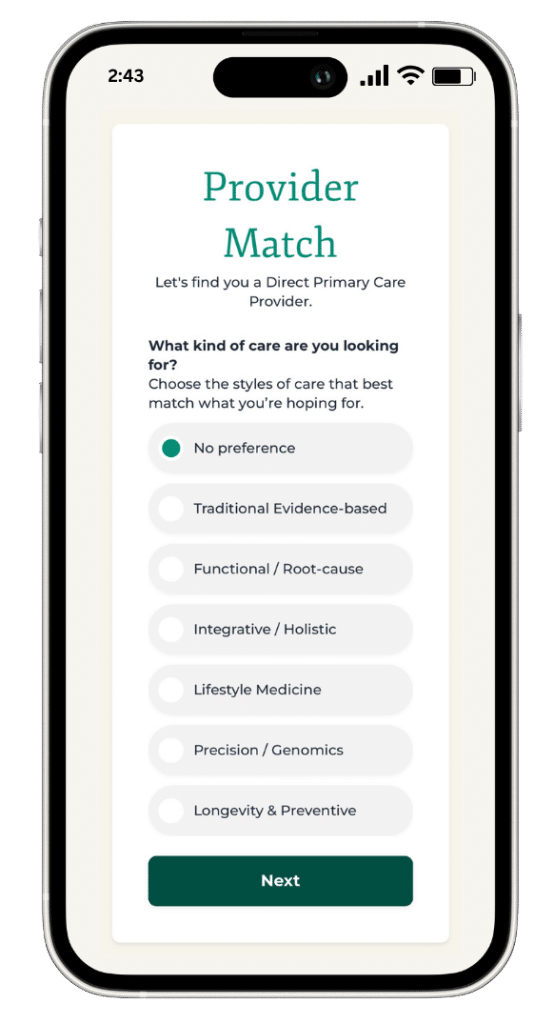
JB: To start, we’re using technology to match each member with the right provider based on their location, care needs, and specific health care preferences. While we carefully vet every provider to make sure they’re excellent primary care physicians, this step helps ensure each person is paired with someone who fits them personally. That is how you build strong, long-term primary care relationships that actually work.
We’re also using technology to bring the kind of cost-saving services that are usually reserved for large corporate health plans to everyone. For example, when someone needs care beyond their core membership, like an MRI, we can help them find high-quality, low-cost options in their area. An MRI through a hospital system might cost two or three thousand dollars, but we can help members get the same quality for around five hundred dollars or less. The same is true for lab work, specialist visits, and other needs outside of the core membership.
It’s not live yet, but we’re building a platform to help members access medications at or near wholesale prices. That can mean 80 to 90% savings compared to what it might cost through insurance or at retail pharmacies.
Broadly, our goal is to use technology to make what’s often a manual and expensive process more affordable and accessible. These tools bring the kind of support usually reserved for high-cost concierge care or large employer plans to everyone, while helping doctors focus on patient care instead of admin work.
RG: How much is a monthly membership?
JB: We just launched our new site with the updated structure. https://aloehealth.co/pricing/
The core membership is $125 a month. This is unlimited access to in-person, virtual, and text-based care with no copays or deductibles.
The Aloe Health+ membership starts at $196/mo. That includes the core membership and adds access to a health-sharing community that helps manage medical expenses beyond our enhanced primary care model.
RG: A new federal policy has changed how people can pay for primary care, creating fresh opportunities for reform. The recent legislation around direct primary care represents a major shift in what’s possible. Can you break down what this means for individuals and employers, and why it’s such a pivotal moment for health care access?
JB: This new federal policy really changes the equation for how people can access primary care. Historically, if you had a high-deductible health plan and an HSA, the message was you have insurance, but you are still paying out of pocket for everything until you hit a big deductible. And even worse, it is often the very people who cannot afford that deductible who are stuck on high-deductible plans in the first place. That pushed a lot of people to delay care. About 40 percent of people are currently forgoing care because of the cost.
Now, for the first time, individuals and employers will be able to pair a direct primary care membership with a high-deductible plan and still use HSA dollars for it. That means you can have real access to your doctor without worrying about deductibles or copays. It fixes one of the biggest gaps in our system. The important detail is that this only works when care is delivered through a membership-based primary care model. High-deductible plans no longer have to mean you are on your own until you hit some astronomically high deductible.
When you zoom out, the potential impact is huge. If we can make this the norm, we finally get to build health care around prevention and long-term health instead of reacting only when something goes wrong. It flips the incentive structure. It puts primary care first. And it gives families and employers a way to get better care at a lower cost, while giving physicians more time and support to actually practice medicine. That is the kind of structural change the system has needed for a long time.
RG: Aloe Health partners with a range of local practices, including some that are faith-based. How does that fit into your broader mission, and how do people choose the type of care model that aligns with their own beliefs or preferences?
JB: I am not saying anything new or earth-shattering when I say that across every part of our lives, expectations for personalization are rising. Whether it is the food we eat, the way we shop, how we learn, or where we work, people want experiences that reflect their values, preferences, and needs. Health care is no different, and it is one of the areas where personalization matters most, yet has lagged behind other industries.
For primary care to really work, you need a relationship with a provider you trust. That is incredibly hard to build inside the traditional system, where doctors are rushed, overwhelmed, and often pushed into a one-size-fits-all model. Membership-based care changes that. It allows practices to form deeper relationships with their members, and it gives them the freedom to build a practice around a specific focus or philosophy.
Today, you see membership-based practices specializing in different health care needs and care philosophies. On the needs side, it might mean a focus on women’s or men’s health, certain chronic conditions, LGBTQ+ care, or different life stages, among other things. On the preference side, it might mean faith-based care, a longevity-focused approach, or a holistic model.
Of course, with that flexibility comes a new challenge. You still want to know the person you choose is highly qualified, aligned with your needs, and the right fit for your family. And you also want to make sure that care connects to all of your other health care needs. That is where we come in. We help people identify what matters most to them in a primary care relationship, and then we match them with high-quality physicians who fit those needs. We intentionally partner across different practice styles and care philosophies because people are not one-size-fits-all, so their care should not be either.
We want to make sure you can find the provider who feels right for you, and then build your entire health care experience around that personalized relationship.
RG: As health care continues to evolve, technology, transparency, and trust are becoming inseparable. What’s next for Aloe Health, and how do you see membership-based primary care shaping the future of accessible, people-centered health care?
JB: We really believe that easy access to membership-based primary care, with no copays or deductibles, is the foundation for great health care. Everything starts there. As I said before, the other reason this matters so much is that it flips the incentive model and aligns our incentives with those of our members. So everything we do starts with that foundation.
From there, we get to do some really interesting things across the whole health care experience. For example, we can help people save up to 90% on medications, save thousands on MRIs, and navigate to better specialists. All of that becomes possible because of what we are doing at the primary care level.
And as we look at what is happening in the ACA marketplace, with people seeing their premiums go up significantly for 2026 to totally unaffordable levels, we want to make sure we are supporting those families, too. We are launching Aloe Health+, which pairs our core membership with access to a health-sharing community. We know it is a bit unconventional, but we are trying to find ways we can get people access to better health care that they can actually afford, however that may be.
Source link